Birth injuries are a type of complex medical malpractice claim typically alleging obstetrician or gynecologist negligence during vaginal delivery, improper induction of labour, cesarean delivery complications, or any straying away from the guidelines and standard of care set forth by the American College of Obstetricians.
Here are the types of birth injury/medical malpractice claims BILA lawyers will accept:
- Injuries Caused by Delayed Delivery
- Failure to Progress During Labor and Delivery
- Oxytocin Use
- Shoulder Dystocia
- Negligence in Antenatal Care
- Negligence in Neonatal Care
- Negligence in C-Section or Operative Delivery
- Death of Mother or Baby
Virtually anything that goes wrong during pregnancy or labour and delivery can raise questions about the quality of medical care and any unforeseen risk factors that an obstetrician failed to promptly recognize and professionally manage.
The only way to know if a malpractice claim exists is to properly investigate the facts and medical-legal issues involved. If you or your family have questions or concerns about the medical care you received during pregnancy or the birth of your child, a BILA lawyer will be able to advise you of your legal rights and whether a birth injury claim should be advanced.
Each vaginal birth and Cesarean section has its own particular set of facts and challenges that uniquely sets it apart from others. It would, therefore, be impossible to describe every single scenario that might give rise to a birth injury claim, but on this page, we’re going to discuss the following common scenarios:
- Shoulder dystocia and improper McRoberts maneuvers
- Brachial plexus injuries
- Macrosomia
- Episiotomy complications
- Suprapubic pressure and anterior shoulder complications
- Erb’s Palsy
- And much, much more…
If you have any questions or concerns regarding a potential birth injury claim or your obstetrician’s management of shoulder dystocia during a vaginal birth or Cesarean delivery, it’s absolutely imperative that you contact us for a free consultation so we can review your case for any gynecology errors and help you better determine what your legal options are.
A. Cerebral Palsy and other Neurologic Injuries Caused by Delayed Delivery
Sadly, a common type of birth injury claim is one involving neurological injury and brain damage to a newborn that was ultimately caused by an obstetrician’s team (doctors, nurses, midwives) failing to intervene or expedite delivery in the face of blatant risk factors associated with fetal distress.
If the baby is incapable of tolerating the birth canal environment for whatever reason, an urgent delivery by Cesarean section or other emergency vaginal delivery maneuvers like a cephalic replacement, an episiotomy may be necessary.
The failure to deliver the baby promptly in these circumstances can lead to the following:
- Oxygen deprivation, a condition known as hypoxia or asphyxia
- Risk of shoulder dystocia
- Permanent brachial plexus injuries (Brachial plexus palsy)
- Erb’s Palsy
- Umbilical cord compression
- As well as many other common birth injuries…
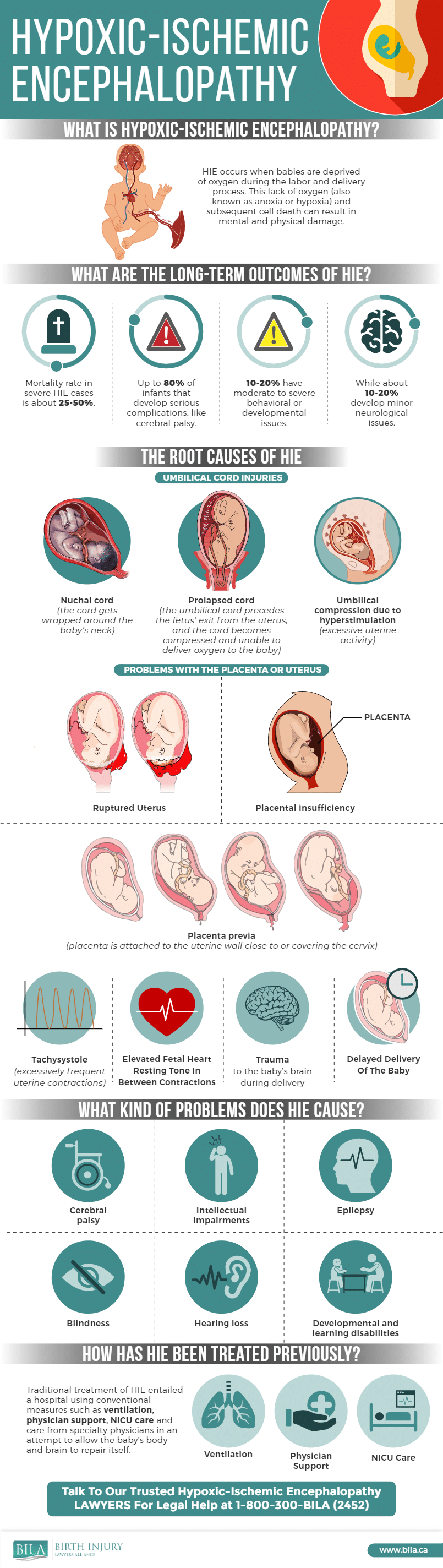
Here is an infographic describing HIE:
Severe or prolonged hypoxia/asphyxia can lead to a significant decreased blood supply to the baby’s organs, called ischemia, and can result in permanent brain damage and other injuries to a newborn’s vital organs.
Hypoxic-ischemic encephalopathy or HIE is a condition involving injuries to a baby’s brain caused by a lack of oxygen (“encephalopathy” simply means brain sickness). Babies with these types of injuries may later develop permanent neurologic conditions such as cerebral palsy (CP) or other cognitive and developmental problems.
Although CP has a variety of other causes, a significant number of CP cases, in absolute terms, can be attributed to impaired oxygenation during labour and vaginal delivery.
A number of factors can lead to this type of injury. These include, but are not limited to:
- Umbilical cord compression;
- Fetal macrosomia and other large baby complications
- Abnormal uterine contractions, particularly those occurring too frequently or lasting too long;
- Shoulder dystocia, including posterior shoulder and complications involving the delivery of the posterior arm
- Low blood pressure in the mother (maternal hypotension):
- Uterine rupture;
- Placental abruption;
- Excessive pressure on the baby’s head during uterine contractions, as well as suprapubic pressure and fundal pressure.
The obstetrician’s team is charged with monitoring fetal and maternal well-being throughout the induction of labour and delivery. They can monitor the baby’s well-being using a variety of surveillance techniques, including electronic fetal heart monitoring (EFM). EFM will invariably give clues about how the baby is tolerating the contractions and the stresses of labour. If a baby is deprived of oxygen, this will cause changes in the heartbeat; these changes will be evident on the EFM tracing.
Warning signs on EFM tracings must be heeded by the Obstet Gynecol team. The failure to intervene in the face of worrisome changes and other risk factors on the EFM tracing can result in serious injury to the baby, including HIE. Such medical errors can form the basis of a successful birth injury claim.
BILA lawyers will often accept cases in which the Obstet Gynecol team failed to expedite the delivery despite what should have been apparent concerns from the EFM tracing and other clinical information. In other words, the failure to perform an urgent or emergency Cesarean section or to deliver the baby by other operative means may give rise to a birth injury claim.
B. Failure to Progress During Labor and Delivery
In some cases, a birth injury may occur because the obstetrical team failed to perform or arrange a c-section despite a failure to progress during labour and delivery. Throughout childbirth, the team should monitor dilation of the cervix, the position of the baby and the descent of the baby in the birth canal. If the labour is not progressing at all or is slow to progress, intervention may be necessary in order to prevent neurological injury or even death.
There are a number of reasons why labour and delivery may not progress as expected, such as the baby’s position, size of head, or uterine contractions that are too weak to push the baby through the birth canal. Regardless of the reason, failure to progress can be dangerous to the health of the baby, and may also harm the mother. For this reason, if an obstetrical team does not appropriately monitor labour and delivery and intervene when medically necessary, a birth injury claim may arise.
C. Oxytocin Use
BILA lawyers frequently handle cases involving the imprudent use of oxytocin. Oxytocin, also known as Pitocin or Syntocinon, is a medication commonly used to initiate or induce labour and expedite delivery. Oxytocin accomplishes this by stimulating the uterus.
Oxytocin also causes the uterus to contract more frequently and with greater intensity, thereby causing more rapid cervical dilatation and descent of the baby in the birth canal. When properly utilized, Oxytocin is a valuable and important tool for the Obstet Gynecol team. Problems arise when too much Oxytocin is used or when the obstetrical team fails to recognize that the Oxytocin is negatively impacting the health of the baby or mother.
As previously mentioned, a normal, healthy baby is usually able to tolerate the stresses of labour, including the stress of uterine contractions. Problems may arise, however, if the contractions become too frequent, a condition known as tachysystole or uterine hyper-stimulation.
Oxytocin is a medication that is known to cause hyper-stimulation of the uterus when used in excess. Too much Oxytocin can result in waves of contractions that effectively reduce the baby’s oxygen supply. Without enough time to recover between contractions, the baby begins to deplete its reserves. If this continues, the baby’s reserves become dangerously low and the baby will decompensate, eventually resulting in a hypoxic-ischemic injury.
Given the potential for oxytocin to hyper-stimulate the uterus, it is imperative that the Obstet Gynecol team carefully administer Oxytocin and monitor the dosage and the mother’s and baby’s response. If there is evidence of uterine hyper-stimulation or worrisome changes on the EFM tracing, Oxytocin should be tapered or discontinued to prevent injury to the baby and the mother.
In addition to the indirect impact of Oxytocin on the baby’s oxygen supply, Oxytocin may also directly result in uterine rupture, a condition that poses a grave risk to mother and baby.
In short, the imprudent use of Oxytocin may form the basis of a birth injury claim, and BILA lawyers are frequently consulted on such cases.
D. Shoulder Dystocia
In a normal vaginal delivery, the baby’s head will emerge first, followed by the shoulders. In some cases, however, one or both shoulders may be trapped beneath the pelvic bone; this condition is known as shoulder dystocia. Without an immediate response by the obstetrical team, shoulder dystocia can lead to serious injury to the baby’s arm and shoulder, or even brain injury and death.
There are a number of risk factors for shoulder dystocia, including a petite mother, gestational diabetes, and a baby who is large for their gestational age. In these cases, the obstetrical team should be prepared for the possibility of a difficult vaginal delivery. There are certain manoeuvres that can be done to free a baby’s shoulders from the pelvic bone. If these manoeuvres are not done, or if an alternative (such as a c-section) is not recommended, then these failures may form the basis of a birth injury claim.
E. Negligence in Antenatal (Prenatal) Care
Beyond labour and delivery, obstetrical malpractice may also occur over the course of a pregnancy. Obstetricians have a duty to properly monitor expectant mothers during pregnancy, and to manage any issues that may arise. Proper antenatal (prenatal) care includes monitoring and screening both the mother and baby throughout the pregnancy.
Physicians should carefully monitor maternal blood pressure and glucose levels, perform fetal surveillance, and assess the health of the baby through blood tests, ultrasonography, and heart rate monitoring (EFM). In addition, genetic testing and amniocentesis may be warranted in certain cases. A failure to perform these tests or otherwise care for an expectant mother and baby may be considered negligent antenatal care.
F. Negligence in Neonatal Care
BILA lawyers also accept cases involving substandard neonatal care, which involves the care a baby receives after delivery. Depending on the baby’s condition at birth, a wide range of care requirements may come into play. If the delivery was difficult or complicated, a neonatal team may be required to resuscitate and treat the baby immediately at birth. The failure to have that team present at the time of delivery may raise questions about the quality of care.
A baby who is born after a difficult delivery may require ongoing care in a critical care setting such as a neonatal intensive care unit (NICU). The baby may require an ultrasound, CT or MRI brain imaging, or may require being transferred to a pediatric hospital.
If the baby has suffered a hypoxic-ischemic brain injury, treatment with hypothermia (cooling) and other forms of management may be necessary to minimize the harm. Should the baby develop seizures, these will need to be quickly treated to avoid further neurological injury.
All of these very complex issues may be the subject of a birth injury claim.
G. Negligence in C-Section or Operative Delivery
A variety of problems can occur during a Cesarean section or operative delivery (i.e. forceps, vacuum). In some cases, the outcome from the operative delivery may raise questions that warrant investigation by a BILA lawyer.
A negligently performed Cesarean section may result in injuries to the mother, including injuries to her bladder, uterus, blood vessels and other vital organs. Lacerations and injuries to the baby are also possible.
Delivery by forceps likewise carries risks to both mother and baby. Negligent use of forceps may result in injuries to the mother’s bladder, urethra, and perineum. Risks to the baby include cranial fracture, facial fracture, and lacerations or injuries to the facial nerves. In rare cases, the baby may suffer brain damage or death.
H. Death of Mother or Baby
In some cases, the process of labour and delivery, or complications during pregnancy, may result in the death of the mother or baby.
These heart-wrenching cases usually involve the same issues seen in cases of maternal or fetal injury. The issues of standard duty of care and causation must be investigated in order to determine if a valid malpractice claim exists.
Contact Our Team of Birth Injury Experts For More Information About Holding Negligent Obstetricians and Gynecologists Accountable
Our team of experienced birth injury lawyers has helped countless clients in terms of successfully navigating and executing all types of birth injury claims.
We are confident that we can help anyone who has suffered from medical malpractice throughout prenatal care, labour, delivery, and neonatal care.
Contact us today for a free consultation so we can review the facts pertaining to your birth injury claim, and begin initiating the necessary first steps towards holding any negligent parties accountable.
- Long Term Effects of a Nuchal Cord - May 6, 2022
- Greatest Risks for Cerebral Palsy Occur Prior to Birth - August 28, 2020
- Alberta to Begin Screening Newborns for Four New Conditions - September 27, 2019