Oxygen Deprivation During Labour and Delivery
The medical term is hypoxic ischemic encephalopathy (HIE). This simply means brain sickness from inadequate oxygenation to the brain. The fetus receives his or her necessary oxygen and nutrients from the mother through the umbilical cord. If this mechanism of delivery of oxygen and nutrients is compromised the fetus may suffer an irreversible neurological injury.
Hypoxic Ischemic Encephalopathy, or HIE, occurs when an infant’s brain is deprived of oxygen during the birthing process. Simply put, HIE, or oxygen deprivation during labor and delivery, occurs because the fetus no longer receives adequate oxygen during delivery, often because the blood flow between mother and fetus through the umbilical cord is cut off.
Hypoxia, or low oxygen in the tissues, can result in hypoxic-ischemic injury which can lead to long-term disabilities and challenges for the infant and their family.
Quick Information about HIE
The Long-Term Impact of HIE
Oxygen deprivation during birth can lead to a number of lifelong impacts on the child’s development, including severe brain injury, which may mean challenges ranging from low APGAR scores immediately after birth to long-term neurodevelopmental challenges. Even mild HIE can have severe consequences for the entire family.
- Cerebral palsy. Cerebral palsy is a general name for a group of disorders that may include exaggerated reflexes, floppy or rigid limbs, atypical muscle tone, and involuntary movements often as a result of brain damage during development or birth. Up to 80% of oxygen-deprived infants may suffer from serious complications like cerebral palsy.
- Neurological, behavioral, and developmental issues. Children who suffer birth asphyxia may have moderate to severe behavioral or developmental issues. Some children may suffer from other neurological issues. Often, the central nervous system is significantly impacted by HIE. HIE can impact all infants, from term infants delivered at 40 weeks to preterm infants. Regardless of the infant’s age, it’s critical to follow up with neurology and ensure that infants who sustained oxygen deprivation during birth are closely monitored and receive appropriate pediatric interventions, since they may have considerable intellectual impairments or learning disabilities as a result of ischemic brain injury.
- Sensory challenges. Infants who suffered oxygen deprivation during birth may suffer from vision or hearing loss. Sometimes, these abnormalities and challenges may be clear during the early days of life; other times, parents may need more time to notice these problems.
- Seizures. Infants who suffer from HIE may show signs of subtle seizure activity shortly following birth and may also have a high risk of developing seizures later in life.
Causes of HIE
Contractions during labour result in a reduction of blood flow through the umbilical cord and thus a reduction in the delivery of oxygen and nutrients to the fetus. When the contraction ends, the blood supply through the umbilical cord usually returns to normal. In the vast majority of situations, the fetus can tolerate the momentary reduction in blood supply during a contraction and recovers during the resting phase in between contractions.
In some cases, however, the repeated reduction in the supply of oxygen and nutrients during contractions will exceed the reserves of the fetus and, if this pattern continues, can result in neurological injury. Fetuses that are growth restricted, or are preterm, have lower reserves and are therefore less able to tolerate the reduction in blood supply with contractions.
If labour is induced or augmented with oxytocin this can cause the contractions to be more frequent and longer, reducing the time between contractions and limiting the fetus’s ability to recover. There can be a transfer of blood between twins (referred to as twin-to-twin transfusion) that reduces the ability of the twins, or one of them, to tolerate the stress of labour.
Contact Us Today
Contact us today to learn more about how our birth injury lawyers have helped families provide for their children and receive peace of mind.
Here is an infographic describing HIE:
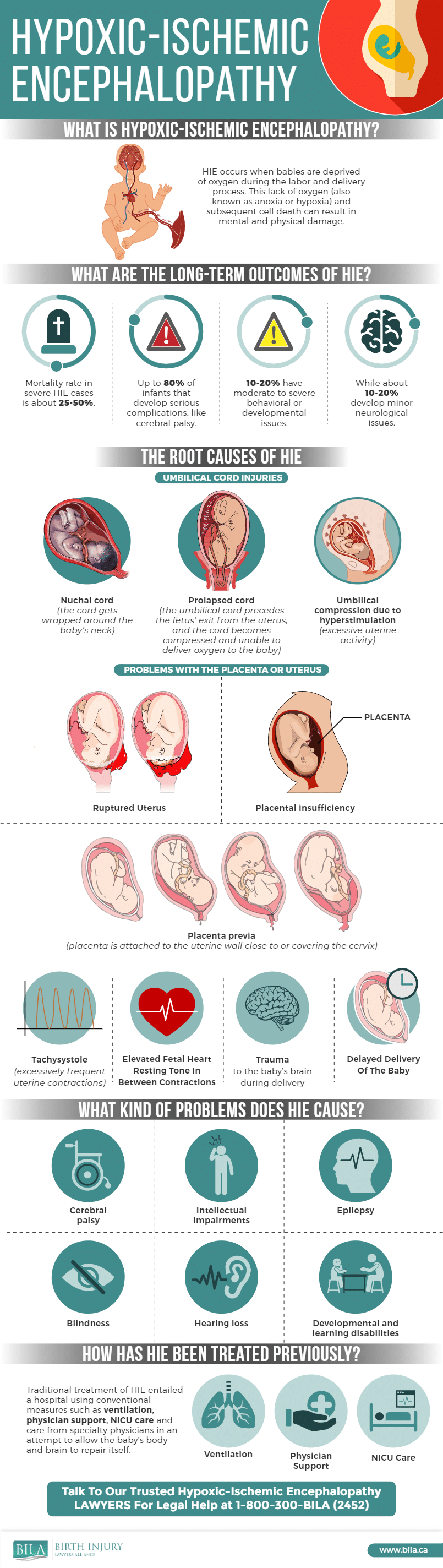
Common complications that can lead to HIE include:
- The umbilical cord around neck of the infant during the childbirth process (also known as a nuchal cord).
- The umbilical cord becomes prolapsed or exits the uterus ahead of the baby, which can cause it to compress too much to deliver sufficient oxygen to the baby.
- Excessive compression of the umbilical cord, often caused by excessive uterine contractions, high material blood pressure, or complications during delivery.
- The placenta detaches too early (placental abruption) or is insufficient–that is, fails to provide necessary nutrients and oxygen to the infant.
- The mother suffers from placenta previa (a condition where the placenta blocks the cervix), which can cause serious problems as the cervix dilates and labor progresses. Mothers with full placenta previa usually have a C-section to help protect fetal and maternal health.
- The uterus ruptures during delivery, which may lead to maternal hemorrhage and cut off blood flow to the baby. This is more common following a previous cesarean section.
- The baby’s brain suffers trauma during delivery, sometimes as a result of forceps use, dropping the infant, or otherwise applying excessive force on the baby’s head.
Often, the HIE can be avoided with appropriate monitoring and medical intervention before the child suffers excessive oxygen deprivation.
Health care providers may observe warning signs, including elevated fetal heart rates or falling heart rate during the labor and delivery process. In those cases, they must often act very quickly to avoid serious injury.
Treatment for HIE
A baby who has suffered significant oxygen deprivation during labour will often require extensive resuscitation at birth. The timing and procedures used to resuscitate the baby can have a significant effect on whether or not the baby suffers a permanent brain injury, or on the extent and impact of the brain injury.
Further, a baby born with HIE will benefit from whole body cooling, or therapeutic hypothermia.
See More on HIE Treatment
Can HIE be Avoided?
One of the responses of the fetus to the decrease of blood flow with contractions is a change in the fetal heart rate and its pattern. Thus, the theory behind electronic fetal monitoring is to detect any changes in the fetal heart rate or pattern that suggests that the fetus is not tolerating labour and to allow for intervention prior to the neurological injury occurring. It is the responsibility of both nurses and doctors to respond to any evidence of impaired fetal oxygenation suggested on the fetal heart tracing. By doing so, injury to the baby can, in some circumstances, be avoided or mitigated.
There are also situations where the fetal blood supply is suddenly and significantly decreased. This can occur with uterine rupture during an attempt at vaginal birth after cesarean, cord prolapse, placental abruption, and shoulder dystocia. This profound decrease in the blood flow will result in a profound decrease in the fetal heart rate which is a sign that the baby will need to be delivered immediately.
- Common Problems in the NICU - March 13, 2024
- Financial Assistance for NICU Stay - June 2, 2022
- Most Common Signs of Fetal Distress in Babies - February 1, 2022

